The pattern and distribution of brain injury provide important information which, in combination with the labour and delivery records, allows us to work backward to figure out how and when a baby was injured. Importantly, it also helps to predict what parents can expect for their child’s recovery and quality of life. These injuries are detected with neuroimaging of the newborn brain (ultrasound, CT scan, and MRI).
There are essentially two main patterns of newborn brain injury that are caused by birth trauma. Those patterns of brain injury are the so-called “Watershed” injury and deep grey matter injury.
A Quick Word About Neuroimaging And HIE
Neuroimaging is essential to the diagnosis and treatment of newborn brain
illness, or hypoxic ischemic encephalopathy (HIE). These investigations play a crucial role in establishing the nature, extent and timing of a baby’s brain injury. Armed with this information, doctors are increasingly able to tailor their treatment and rehabilitation regimens to address the individual needs of children who have suffered birth trauma.
Neuroimaging studies are likewise crucial in establishing a legal case for obstetrical malpractice.
Recent medical research involving MRI technology has shown that a significant proportion of injured newborns suffer their brain injury at or near the time of birth. MRI is the most sensitive tool for assessing brain injury in the newborn. While a cranial ultrasound in the first 24-72 hours of a baby’s life will provide important information about the onset of brain swelling, an MRI on day seven of life and later (after the initial brain swelling has subsided) will provide critical details that show the extent and nature of the baby’s brain damage.
Advanced MRI technology, particularly something known as the Diffusion
Weighted MRI (DW-MRI) is actually even more sensitive than conventional MRI and is proving to be useful even in the first hours and days of life. Finally, unlike CT scans, MRI technology does not expose the baby’s brain to radiation, which is an important consideration.
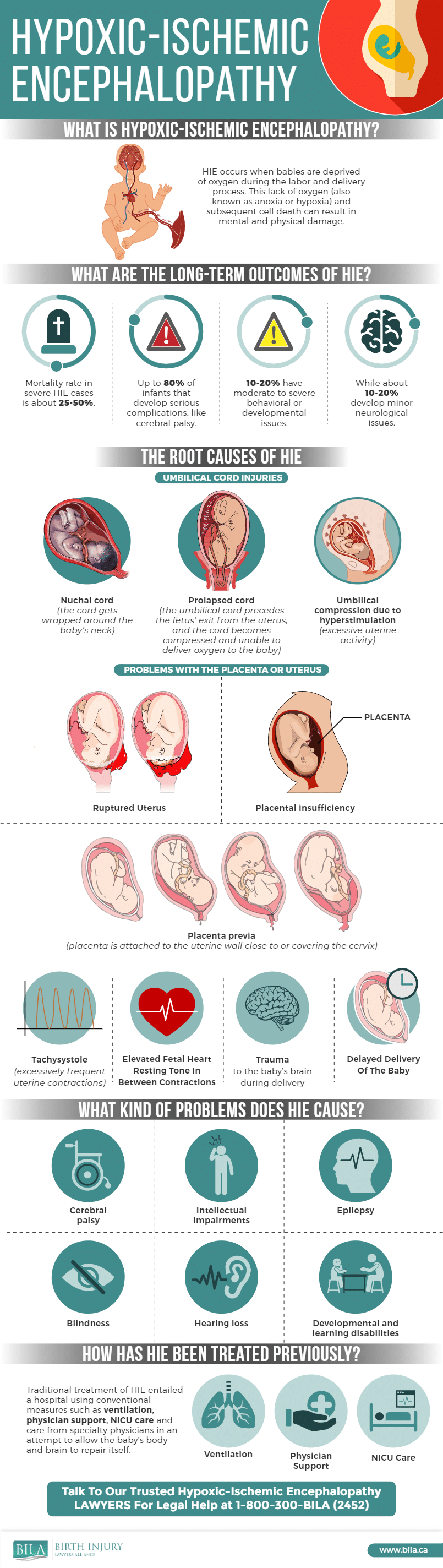
Here is an infographic describing HIE:
The Two Characteristic Patterns of Brain Injury in HIE
As previously mentioned, HIE is generally associated with two specific patterns of brain injury in a full term newborn. One is the watershed injury; the other involves injury to deeper brain structures.
1. The Watershed Injury
The Watershed affects the areas of the brain that are supplied by the anterior middle cerebral artery and the posterior middle cerebral artery. These anatomical regions, found in both hemispheres of the brain, are referred to interchangeably as the “watershed zones,” the “border zones,” or the “parasagittal zones.” These areas are composed of both white matter and grey matter in the cortex of the brain. The cortex is the wrinkly, outermost layer of the brain.
White matter consists of bundles of myelinated axons and is the “conductor” of electrical impulses between different areas of grey matter in the brain. Grey matter is composed of the actual neurons (nerve cell bodies) which are capable of generating and maintaining the electrical impulses/signals that are the basis for the proper functioning of the nervous system.
A Watershed injury, therefore, involves damage to the so-called watershed
zones. This injury pattern most commonly affects only the cortical white matter in the watershed zones on both hemispheres of the brain, but if a baby is deprived of oxygen for long enough, this can also lead to injury to the grey matter in the cortex of the brain (cortical grey matter).
2. Injuries to Deeper Brain Structures
In the event of a total or near-total deprivation of oxygen or a particularly severe prolonged partial hypoxia, the fetus may suffer damage to the deeper gray matter structures of the brain, including the basal ganglia and thalami. These structures are typically injured by acute (also referred to as “sentinel”) events such as placental abruption, severe umbilical cord compression, umbilical cord prolapse, and uterine rupture, all of which can result in a sudden and profound decrease in oxygen to the fetus.
The basal ganglia and thalami have a relatively high oxygen demand so that
when there is a total or near-total deprivation of oxygen, these deep structures will suffer injury in relatively short order, often within minutes. This stands in contrast with a prolonged partial deprivation of oxygen which the baby can often tolerate for hours without causing serious injury.
It is important to note that there are many cases where both patterns of injury will occur. This mixed pattern of injury can be seen when there is both a severe prolonged partial asphyxia and a total or near-total asphyxial event during labour.
What Can I Expect if My Baby has a Watershed Injury?
While it is impossible to predict with certainty the outcome or prognosis for a newborn with a Watershed injury, medical studies have begun to shed light on what parents can expect in these cases.
A general principle that has emerged from the scientific literature is that injuries to the deep brain structures (basal ganglia and thalami) are associated with the most severe long-term impairments of both motor and cognitive function, whereas children who have sustained isolated Watershed injuries (i.e., without the involvement of the deep brain structures) may experience only cognitive deficits, although injury to these structures can cause cerebral palsy.
More recently, medical researchers have discovered that children with
Watershed injuries were more likely to have cognitive deficits that cause lower verbal IQ. This is a very specific type of cognitive deficit. In other words, we are beginning to learn that it is not just the severity of the brain injury that will determine a child’s long-term outcome, but more specifically, the pattern of injury can actually tell us something about the likely pattern of cognitive dysfunction as well.
In children with isolated Watershed injury, that specific pattern of cognitive
dysfunction appears to include language skills, i.e., speech and verbal IQ. On the other hand, researchers have not yet been able to establish an association between isolated Watershed injury and non-verbal cognitive abilities such as visual memory and executive function.
Non-verbal cognitive deficits are, however, observed in children who have mixed patterns of brain injury, i.e., both to the watershed and deeper structures of the brain. As a result, it has been suggested that it is the “interaction” between these two distinct patterns of brain injury that gives rise to non-verbal cognitive deficits.

John McKiggan, QC has represented clients in pediatric and adult injury claims that have resulted in multi-million dollar awards. In recognition of his accomplishments, John has been honoured by his peers, who elected him president of the Atlantic Provinces Trial Lawyers Association. He has also been named Queen’s Counsel, a designation recognizing exceptional professional merit. John has been selected for inclusion in the Best Lawyers in Canada in the field of personal injury law, he is listed in the Canadian Legal Lexpert Directory and has been named a local litigation star by Benchmark Litigation Canada.