Learn more about whole body cooling treatments for babies
- What is Whole Body Cooling?
- How HIE Effects Brain Cells?
- How Does Cooling Therapy Work?
- Does Cooling Help HIE?
- Why Would a Newborn Need to Be Cooled?
- Cooling as Treatment for HIE
- Criteria for Cooling Therapy as Treatment
- What Happens After an Infant Receives Hypothermic Therapy?
During labour and delivery, an infant may suffer oxygen deprivation (hypoxia) and limited blood flow to the brain. This condition, known as hypoxic-ischemic encephalopathy (HIE), is a type of birth injury that can cause permanent brain damage. Infants with HIE may later develop cerebral palsy, cognitive disabilities, seizures, hearing and vision impairments, developmental delays, and other neurological conditions.
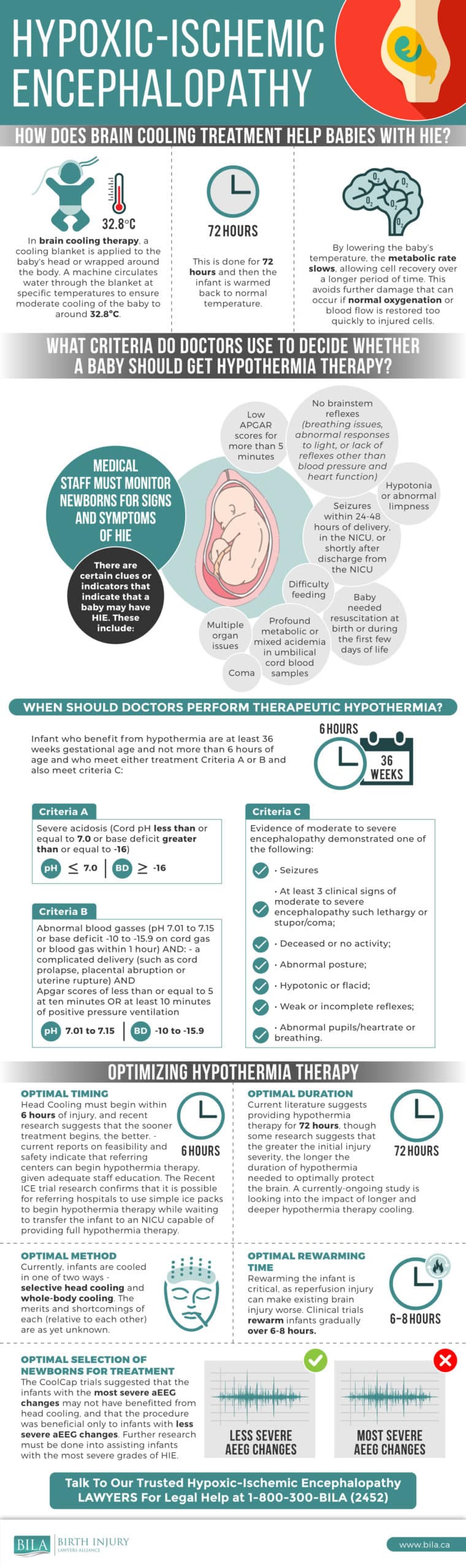
There is one treatment that may be able to minimize permanent brain damage in a newborn due to HIE. Therapeutic hypothermia, or whole-body cooling, involves cooling the baby down to a body temperature of about 32.8° Celsius to help the brain recover from a hypoxic-ischemic injury. When done promptly, within 6 hours after a birth injury, whole-body cooling has the potential to reduce the incidence of death and disability substantially.
What if your child has suffered moderate or severe HIE? In that case, whole-body cooling may be a viable option to minimize the potential disabilities that your baby may suffer due to this birth trauma.
Whole-body cooling is primarily performed in a hospital’s neonatal intensive care unit (NICU). The NICU will have the necessary equipment to properly perform therapeutic hypothermia, which can help to reduce the damage caused by HIE. Below, we explain what to expect when it comes to the NICU cooling protocol.

What is Whole Body Cooling?
Within the last number of years, there have been significant advances in the knowledge and use of head and whole-body cooling to reduce the extent of brain injury associated with a hypoxic-ischemic event (an inadequate supply of oxygen to the brain) and birth injuries.
Those healthcare professionals that practice obstetrics, and physicians who care for newborn children, have an obligation to remain current with these medical developments, to be aware of the inclusion criteria and to have appropriate systems in place to ensure the effective referral and transport of newborn babies who might benefit from whole-body cooling to the appropriate neonatal intensive care unit.
How HIE Effects Brain Cells
A hypoxic-ischemic event during labour can result in a brain injury through two mechanisms. The first is often referred to as the primary insult and refers to the death of the brain cells associated with the hypoxic-ischemic event itself. The secondary insult, which can also result in the death of brain cells, occurs with the swelling of the brain in response to the initial insult. This swelling starts approximately 6 hours after the initial insult. It is these 6 hours that give healthcare professionals time to cool the newborn, which in turn reduces the swelling and the extent of the secondary insult.
It is, therefore, essential that healthcare providers know the inclusion criteria and carefully analyze the clinical situation to determine whether the newborn falls within the criteria. The current criteria require that the baby be more than 35 weeks gestation, weigh more than 1,800 grams, have evidence of a hypoxic-ischemic event during labour based upon an analysis of the blood from the umbilical cord and that the cooling process can begin before 6 hours of age.
There have been some exciting new developments in the area of the head and body cooling with some very good results. Healthcare providers practicing obstetrics and those in charge of newborns must ensure that they remain current with the latest developments in this area and have appropriate policies in place to ensure that newborns that meet the inclusion criteria receive the care they deserve.

How Does Cooling Therapy Work?
The goal of hypothermia therapy is to reduce the baby’s body temperature to about 32.8° Celsius. This is done in one of two ways:
- Using a cooling cap for selective head cooling; or
- Cooling the baby’s entire body (whole-body cooling). This is performed in the NICU with a special blanket that has water running inside of it. This blanket can either warm or cool the body.
The decision on which method is used is based on several factors, including the protocols and equipment available at the Neonatal Intensive Care Unit (NICU). Check with your local hospitals to find out if they have this intervention capability prior to giving birth there.
Shortly after suffering a hypoxic-ischemic event, a newborn’s body temperature will be lowered to 32.8° Celsius using a cooling cap or cooling blanket. Their temperature will be lowered for a period of 72 hours. After 72 hours, the infant is gradually warmed back to normal temperature over a period of 6 to 8 hours. During this time, you might be able to hold your baby for brief times. The NICU staff will keep you updated based on their protocol for whole body cooling.
For whole body cooling, the NICU staff will put a special thermometer into your baby’s esophagus to monitor their temperature. This device is important because neonatologists and other NICU staff need to know that they are cooling the whole baby, not just their skin. A cord then connects the thermometer to the blanket’s temperature controls. This ensures that the water in the blanket is the appropriate temperature. As necessary, the water will either heat up or cool down to maintain the 32.8° Celsius temperature.
The NICU staff will also place IV lines where the umbilical cord was attached. They will administer fluids and draw blood samples to monitor organ function through these IV lines. Your baby will also be attached to an EEG machine to monitor brain activity.
Does Cooling Help HIE?
This decreased body temperature helps to slow the body’s metabolic rate, allowing cells to recover and preventing the spread and severity of brain damage due to oxygen deprivation. One potential benefit of cooling therapy for newborns is that it reduces the likelihood of reperfusion injury, which occurs when the blood flow is restored too quickly to injured parts of the brain.
Before, during, and after whole-body hypothermia therapy, doctors and other pediatric medical professionals must monitor the baby’s health and intervene as necessary. Throughout the process, doctors may:
- Assess the oxygenation of the baby by analysis blood samples
- Manage acidosis (excessive acid in the blood)
- Test for and treat infections
- Provide respiratory and cardiovascular support if necessary
- Maintain normal glucose and electrolyte levels
- Monitor for seizure activity using an EEG and controlling seizures, particularly during rewarming
- Maintain sedation
- Test for brain function using amplitude-integrated electroencephalography (aEEG)
A failure to appropriately monitor an infant and treat any issues that may arise may constitute medical negligence.
Importantly, not all hospitals are properly equipped to administer therapeutic hypothermia. In this situation, the neonate should be transferred to a children’s hospital with the capacity to provide this type of therapy within 6 hours of birth. Typically, whole body cooling is only administered in a NICU, so if you give birth at a hospital without a NICU, then your baby will likely be transferred to a different facility.
The sooner hypothermia therapy begins, the greater the chance for a more favourable long-term outcome for the baby. Many hospitals begin whole body cooling during neonatal transport. This ensures that your baby gets the necessary treatment as soon as possible while en route to the closest NICU.
For parents, it is important to know that your newborn may look different during this NICU whole body cooling treatment. Their skin may be pale or blotchy and they may feel cool to the touch. They may also shiver and appear to be asleep when they are awake. This is normal for therapeutic hypothermia.
Once treatment is finished, the NICU staff will order a magnetic resonance image (MRI) of your baby’s brain. This test allows the NICU doctors to view the brain’s structure and assess the impact of birth asphyxia. The NICU doctors and neurologist will discuss the imaging tests, the details of your baby’s birth injury, and initial assessments to estimate the physical and/or cognitive challenges that they might face in the future. Whole body cooling cannot cure brain damage caused by HIE, but it can help to stop the brain damage from worsening.

Why Would a Newborn Need to Be Cooled?
Whole-body or head cooling is not indicated for every infant who suffers a birth injury or is diagnosed with HIE. Instead, this type of therapy is only indicated for infants who have been diagnosed with moderate to severe HIE. While the treatment is generally safe, there are some risks associated with therapeutic hypothermia. The neonatologists will determine if a NICU cooling protocol is appropriate given your baby’s specific situation.
Directly after birth, the NICU staff will perform a series of tests to assess your baby’s health. This includes blood work and administration of a test to determine their Apgar score. If your baby shows signs of neurological abnormalities or has any “red flags” in their bloodwork (such as too much acid in the blood), then they may be eligible for whole body cooling therapy.
The qualifying criteria for hypothermia therapy include:
- At least 36 weeks of gestational age;
- No more than 6 hours old; and
- Severe acidosis (cord pH less than or equal to 7.0, or a base deficit greater than or equal to -16); OR
- Abnormal blood gasses, AND a complicated delivery (such as cord prolapse, placental abruption or uterine rupture) AND an Apgar score of less than or equal to 5 at 10 minutes, OR at least 10 minutes of positive pressure ventilation; OR
- Evidence of moderate to severe neonatal encephalopathy as demonstrated by one of the following: seizures; decreased or no activity; at least 3 signs of moderate to severe encephalopathy, such as lethargy or stupor/coma; abnormalities in posture; hypotonic or flaccid; weak or incomplete reflexes; or abnormal pupils/heart rate (bradycardia) or breathing.
If your infant meets these criteria, then NICU cooling therapy may be an appropriate choice to reduce brain damage and permanent disabilities related to asphyxia during birth. The goal is to start cooling as soon as possible – within 6 hours after birth.
Cooling as Treatment for HIE
Clinical studies in the early 2000s started with a consensus on the science of HIE and the effects of cooling. According to a study published in the Journal of Resuscitation in 2008,
“A reduction of body temperature by 2-3 degrees C (which constitutes modest hypothermia) following a hypoxic-ischemic event has the effect of reducing cerebral metabolic and biochemical abnormalities and cerebral injury.”
Neonatal therapeutic hypothermia is a relatively new treatment option in which an infant’s total body temperature is reduced shortly after birth in order to reduce the chances of severe brain damage and slow down disease progression. According to the National Institute of Health, there are quite a few long-term benefits to neonatal therapeutic hypothermia. For instance, children who underwent treatment as infants were more likely to have a higher survival rate at 6-7 years of age.
A separate study published in the New England Journal of Medicine in 2005 found that whole body cooling therapy reduced the incidence of infant death by 13%. In addition, 11% fewer babies who received whole body cooling therapy in the NICU were diagnosed with disabling cerebral palsy, compared to the control group.
Later studies confirmed that whole body cooling led to better outcomes for babies who experienced HIE at birth. According to the TOBY trial, 13% more infants who had therapeutic hypothermia treatment after a HIE event had an IQ of 85 or higher at age 6 or 7 compared to the control group. These studies show that when a NICU whole body cooling protocol is properly administered, it can lead to far better outcomes for the infant.
We created a helpful infographic to better describe the process of HIE Cooling:
Criteria for Cooling Therapy as Treatment
Infants who are at or greater than 36 weeks gestation and who meet the necessary criteria should be “offered” hypothermia. Active cooling can be accomplished by selectively cooling the infant’s head with cooling caps or total body cooling with cold packs or cooling blankets. Careful management of rectal or esophageal body temperature at an optimal range of 34 degrees C, plus or minus 0.5 degrees C, is important.
The optimal duration of treatment was not initially clear, but most practitioners used 72 hours of cooling. At the same time, “re-warming” of the neonate is not without controversy, and care needs to be taken to slowly restore body temperature. Worsening of encephalopathy and seizures have occurred on rewarming and may require re-cooling of the infant. Subsequent studies on the therapeutic effects of controlled hypothermia for infants presenting with symptoms of HIE continue to support the therapy as part of the applicable standard of care.
Given the complexity of whole body cooling treatment, it is critical that it be performed by experienced NICU medical professionals. These experts can assess a newborn to determine if this treatment is appropriate. They can then administer the treatment properly, including appropriately monitoring the newborn during the process and rewarming the baby slowly.
Click here for the full Neonatal Practice Guidelines- Hypothermia for Newborns With Hypoxic Ischemic Encephalopathy
What Happens After an Infant Receives Hypothermic Therapy?
After being diagnosed with moderate to severe HIE, an infant who receives NICU cooling therapy should receive follow-up care through infancy and into later childhood. A range of medical professionals from fields such as neonatology, physiotherapy, occupational therapy, neurology, psychology, audiology, and ophthalmology, may be involved in the child’s care.
More than 30% of infants diagnosed with HIE will develop cerebral palsy or another severe disability. Common impairments may include:
- Cognitive deficits, particularly difficulties with reading, spelling, and arithmetic
- Blindness or severe visual impairment
- Hearing loss
- Behavioural difficulties, including emotional problems and hyperactivity
- Childhood epilepsy
For these reasons, parents of a child who has suffered HIE should follow up with a multidisciplinary team of healthcare professionals to ensure that their child receives the best possible care. While the prompt and proper administration of cooling therapy in the NICU can increase the likelihood of a favorable outcome, many children still suffer long-term effects from HIE and other birth injuries associated with birth asphyxia.
- Common Problems in the NICU - March 13, 2024
- Financial Assistance for NICU Stay - June 2, 2022
- Most Common Signs of Fetal Distress in Babies - February 1, 2022
